By Louis ‘Barok’ C Biraogo — January 27, 2025
IMAGINE a mother clutching her feverish child, racing to a hospital only to find no beds available. This is the reality for millions in the Philippines, where the hospital bed shortage has reached crisis levels. With just 0.5 beds per 1,000 people—a fraction of the WHO’s recommendation—Health Secretary Teodoro Herbosa warns that tripling capacity isn’t just a goal; it’s a matter of survival.
This is not just a story of numbers; it is a story of human suffering. It is about mothers giving birth on hospital floors, families traveling hours to reach the nearest medical facility, and patients turned away because there is simply no room. It is a story of inequality, where the urban elite have access to world-class private hospitals while rural communities, particularly in Mindanao, are left to fend for themselves.
A Crisis in Numbers: The Shocking Reality of the Hospital Bed Shortage
The statistics are alarming. According to the Department of Health (DOH) and the Philippine Institute for Development Studies (PIDS), the national average of 0.5 beds per 1,000 people masks even grimmer realities in underserved regions. In provinces like Occidental Mindoro, Masbate, and Sulu, the ratios plummet to as low as 0.096, 0.05, and 0.15 beds per 1,000 people, respectively. These areas, already burdened by high poverty rates, are caught in a vicious cycle: poor health infrastructure exacerbates poverty, and poverty perpetuates poor health.
The consequences are dire. Patients in critical condition are often turned away or forced to wait for hours, even days, for a bed. Rural communities, where poverty is most acute, bear the brunt of this crisis. Many rely on PhilHealth, the national health insurance program, but the lack of accredited hospital beds in their regions renders their coverage nearly meaningless.
The Urban-Rural Divide: Why Where You Live Determines If You Survive
The uneven distribution of hospital beds is a glaring example of systemic inequality. Metro Manila and other urban centers, home to just 11.9% of the country’s hospitals, boast significantly higher bed capacities, thanks largely to private hospitals catering to wealthier populations. Meanwhile, rural areas, particularly in Mindanao, are left with dilapidated facilities and overworked healthcare workers.
This disparity is not just a matter of geography; it is a matter of life and death. A child in Manila with pneumonia has a far better chance of survival than one in Sulu, where the nearest hospital may be hours away and already full. The lack of accredited beds in underserved provinces further compounds the problem, as patients are often forced to travel long distances for care, incurring costs that push families deeper into poverty.
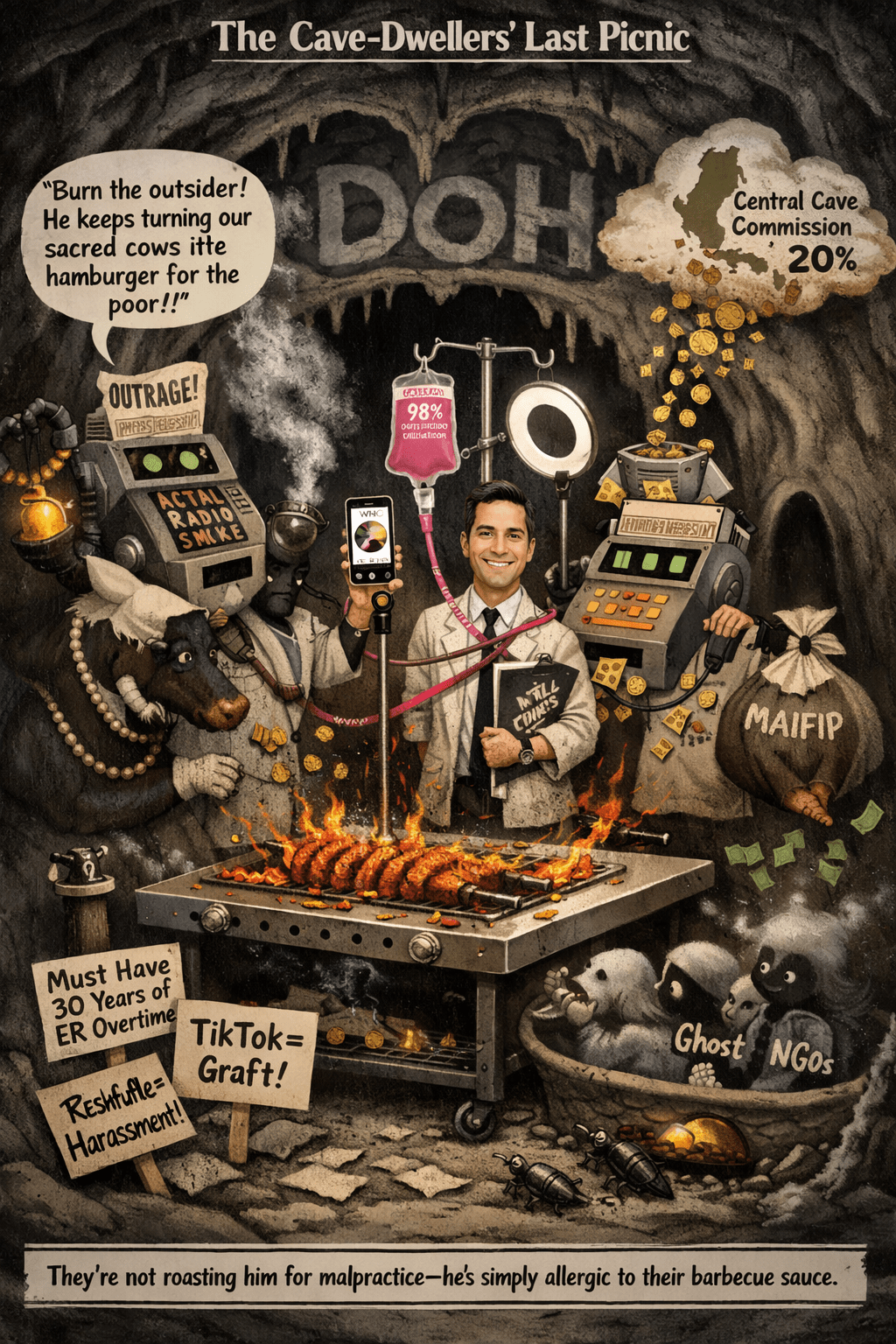
Leading the Charge: The DOH’s Fight to Fix a Broken System
Secretary Herbosa’s call for a tripling of hospital bed capacity is a step in the right direction, but it is only the beginning. The DOH has long struggled to address the root causes of the shortage, including historical underinvestment, market-driven resource allocation, and a lack of strategic planning. While initiatives like the Doctor to the Barrios program have brought much-needed healthcare professionals to rural areas, they are not enough to bridge the gap.
The challenges are immense. Expanding bed capacity requires significant investment in infrastructure, equipment, and human resources. It also requires addressing systemic issues like corruption, inefficiency, and the concentration of resources in urban centers. The DOH must work closely with local governments, international organizations, and the private sector to develop a comprehensive strategy that prioritizes equity and sustainability.
Systemic Failures: Why the Hospital Bed Shortage Runs Deeper Than You Think
The hospital bed shortage is not an isolated problem; it is a symptom of deeper systemic issues. Historical policy decisions, influenced by concepts like Roemer’s Law, have prioritized cost containment over capacity building. Market pressures have further exacerbated the problem, as private hospitals focus on profitability rather than public health needs.
A lack of investment in rural healthcare infrastructure has left entire regions underserved, perpetuating cycles of poverty and poor health. The COVID-19 pandemic exposed these vulnerabilities, as hospitals were overwhelmed and patients were turned away. Without addressing these root causes, any solution will be temporary at best.
Stories of Suffering: The Devastating Human Toll of the Bed Shortage
Behind the statistics are real people—people like Maria, a mother of three from Masbate, who lost her youngest child to dengue because the nearest hospital was full. People like Juan, a farmer from Sulu, who had to sell his land to pay for his wife’s cancer treatment in Manila. These stories are not anomalies; they are the everyday reality for millions of Filipinos.
The human cost of the hospital bed shortage extends beyond individual suffering. It undermines public health, perpetuates poverty, and deepens social inequality. It is a crisis that demands urgent action.
Herbosa’s Crusade: Tackling the Bed Shortage Head-On
Secretary Herbosa deserves credit for bringing this issue to the forefront. His call for a tripling of bed capacity is ambitious but necessary. His emphasis on expanding healthcare access in rural areas, particularly through programs like Doctor to the Barrios, reflects a commitment to equity.
However, his vision faces significant challenges. Expanding bed capacity will require substantial funding, political will, and collaboration across sectors. It will also require addressing systemic issues like corruption and inefficiency. Herbosa’s success will depend on his ability to navigate these challenges and build a coalition for change.
Turning the Tide: Practical Steps to Fix the Bed Shortage
To address the hospital bed shortage, the Philippine government must take bold, decisive action. Here are some recommendations:
- Increase Investment in Healthcare Infrastructure: The government must prioritize funding for the construction and expansion of hospitals, particularly in underserved regions. International organizations and private sector partners can play a key role in providing financial and technical support.
- Promote Equity in Resource Allocation: The DOH should develop a national strategy to ensure that hospital beds and other healthcare resources are distributed equitably. This includes incentivizing healthcare professionals to work in rural areas and expanding PhilHealth coverage in underserved provinces.
- Leverage Technology: Telemedicine and digital bed tracking systems can improve efficiency and reduce the burden on hospitals. The government should invest in these technologies and ensure they are accessible to all Filipinos.
- Strengthen Public-Private Partnerships: The private sector has a critical role to play in expanding healthcare capacity. The government should work with private hospitals to develop innovative solutions, such as portable hospital rooms and emergency bed manufacturing.
- Address Root Causes: The government must tackle systemic issues like corruption, inefficiency, and market-driven resource allocation. This requires political will and a commitment to long-term reform.
Conclusion
The hospital bed shortage in the Philippines is a crisis of access and equity. It is a crisis that demands urgent action, not just from the government but from all sectors of society. Secretary Herbosa’s call for a tripling of bed capacity is a step in the right direction, but it is only the beginning.
As we confront this crisis, let us remember the human stories behind the statistics. Let us remember Maria, Juan, and the millions of Filipinos who deserve better. Let us work together to build a healthcare system that is just, equitable, and capable of meeting the needs of all Filipinos.
The time to act is now. The stakes could not be higher.

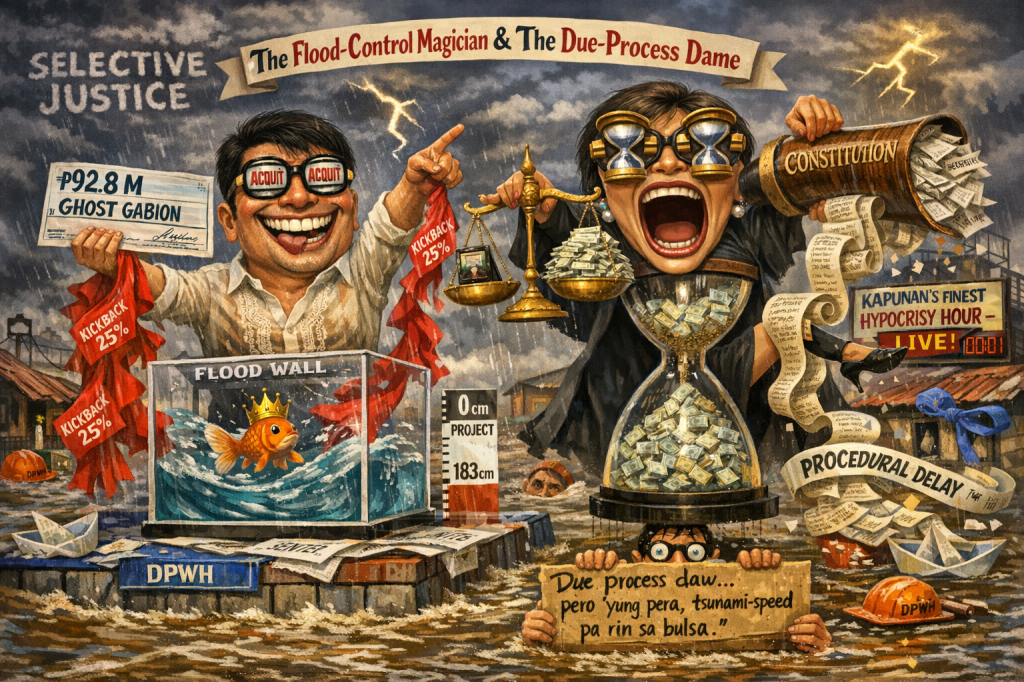
- ₱75 Million Heist: Cops Gone Full Bandit

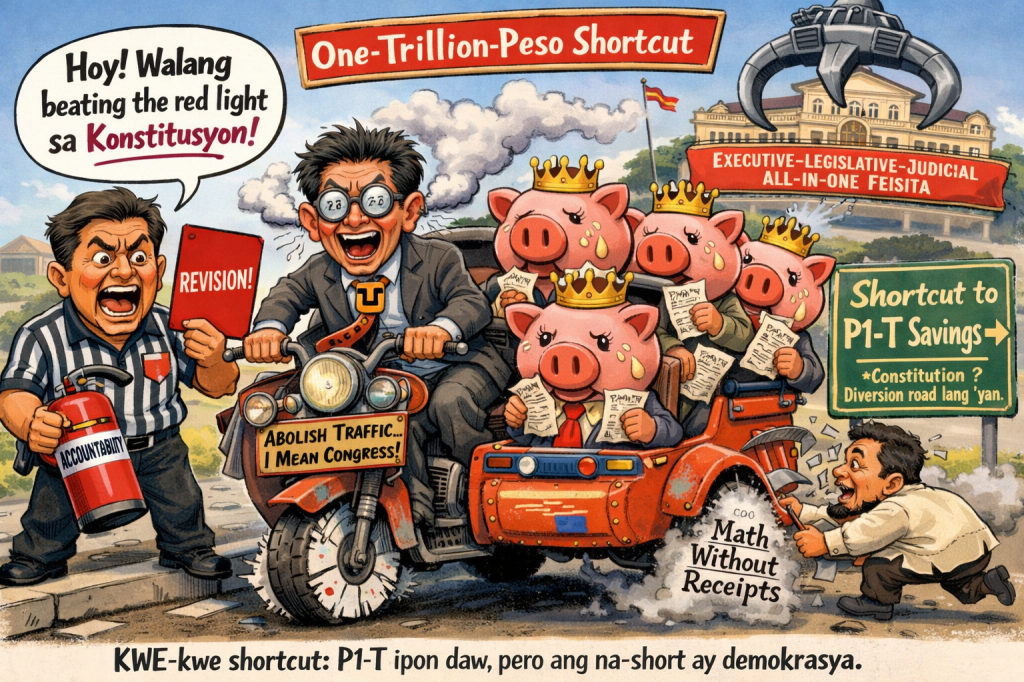
- ₱6.7-Trillion Temptation: The Great Pork Zombie Revival and the “Collegial” Vote-Buying Circus

- ₱1.9 Billion for 382 Units and a Rooftop Pool: Poverty Solved, Next Problem Please

- ₱1.35 Trillion for Education: Bigger Budget, Same Old Thieves’ Banquet

- ₱1 Billion Congressional Seat? Sorry, Sold Out Na Raw — Si Bello Raw Ang Hindi Bumili

- “We Will Take Care of It”: Bersamin’s P52-Billion Love Letter to Corruption

- “Skewed Narrative”? More Like Skewered Taxpayers!

- “Scared to Sign Vouchers” Is Now Official GDP Policy – Welcome to the Philippines’ Permanent Paralysis Economy

- “Robbed by Restitution?” Curlee Discaya’s Tears Over Returning What He Never Earned

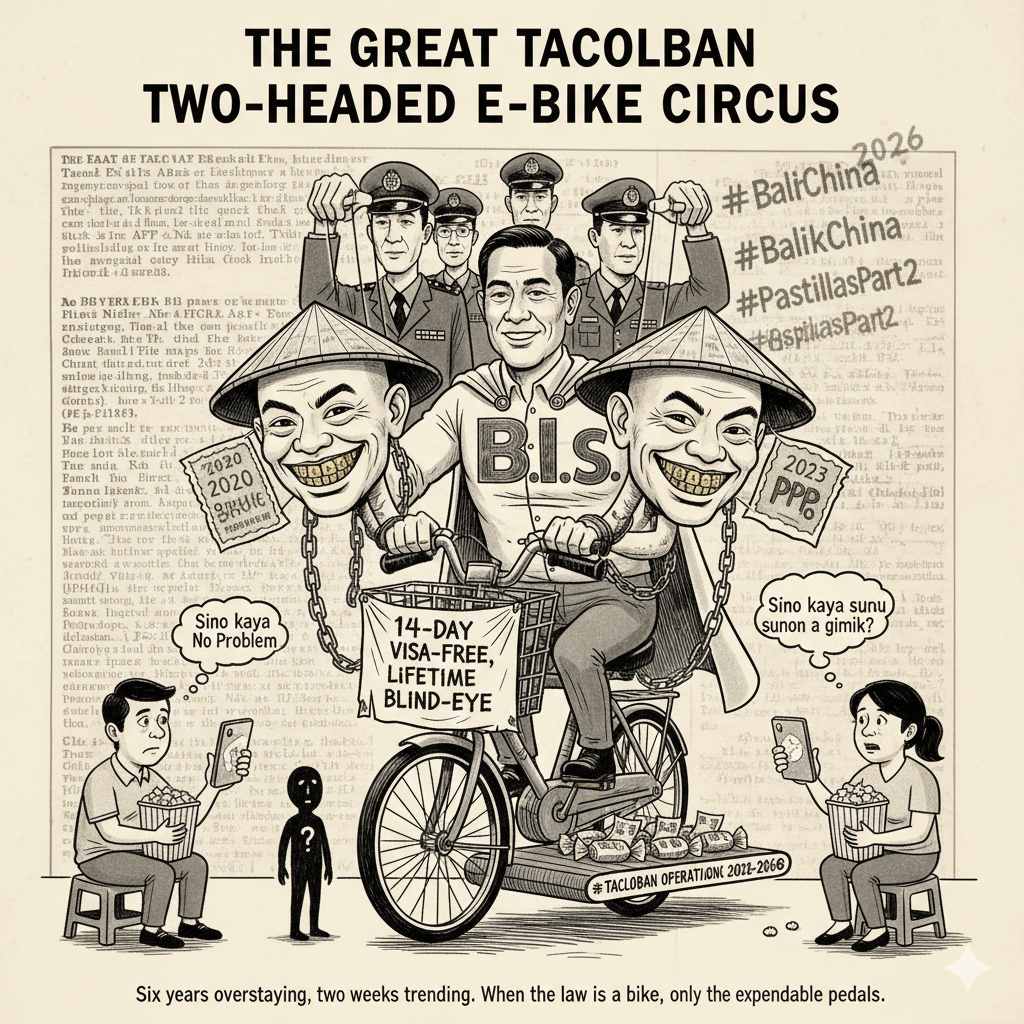
- “My Brother the President Is a Junkie”: A Marcos Family Reunion Special

- “Mapipilitan Akong Gawing Zero”: The Day Senator Rodante Marcoleta Confessed to Perjury on National Television and Thought We’d Clap for the Creativity

- “Bend the Law”? Cute. Marcoleta Just Bent the Constitution into a Pretzel



Leave a comment